Elevance Medicare Journey Strategy
Elevance Health, formerly Anthem, is the largest commercial insurance company in the U.S., but their communications didn’t always reflect their commitment to be more than just a provider. They wanted to connect with people in the run up to their 65th birthdays who were becoming eligible for Medicare to help them take the steps toward enrollment.
The challenge was clear. Healthcare itself is complicated, and Elevance’s prior email messaging had been company-focused rather than considering the enrollee’s needs. The communications were inconsistent, transactional, and didn’t really speak to the actual concerns these audiences were carrying. People weren’t just wondering which plan was right for them; they were wondering if they could trust this brand with their health.
Adding to the complexity, Elevance had limited demographic data on these audiences. Personalization had been more guesswork than strategy. They needed a strategy rooted in empathy, and a communication journey that understood enrollees deeply and helped them feel reassured.
Before we could guide them, we needed to know them.
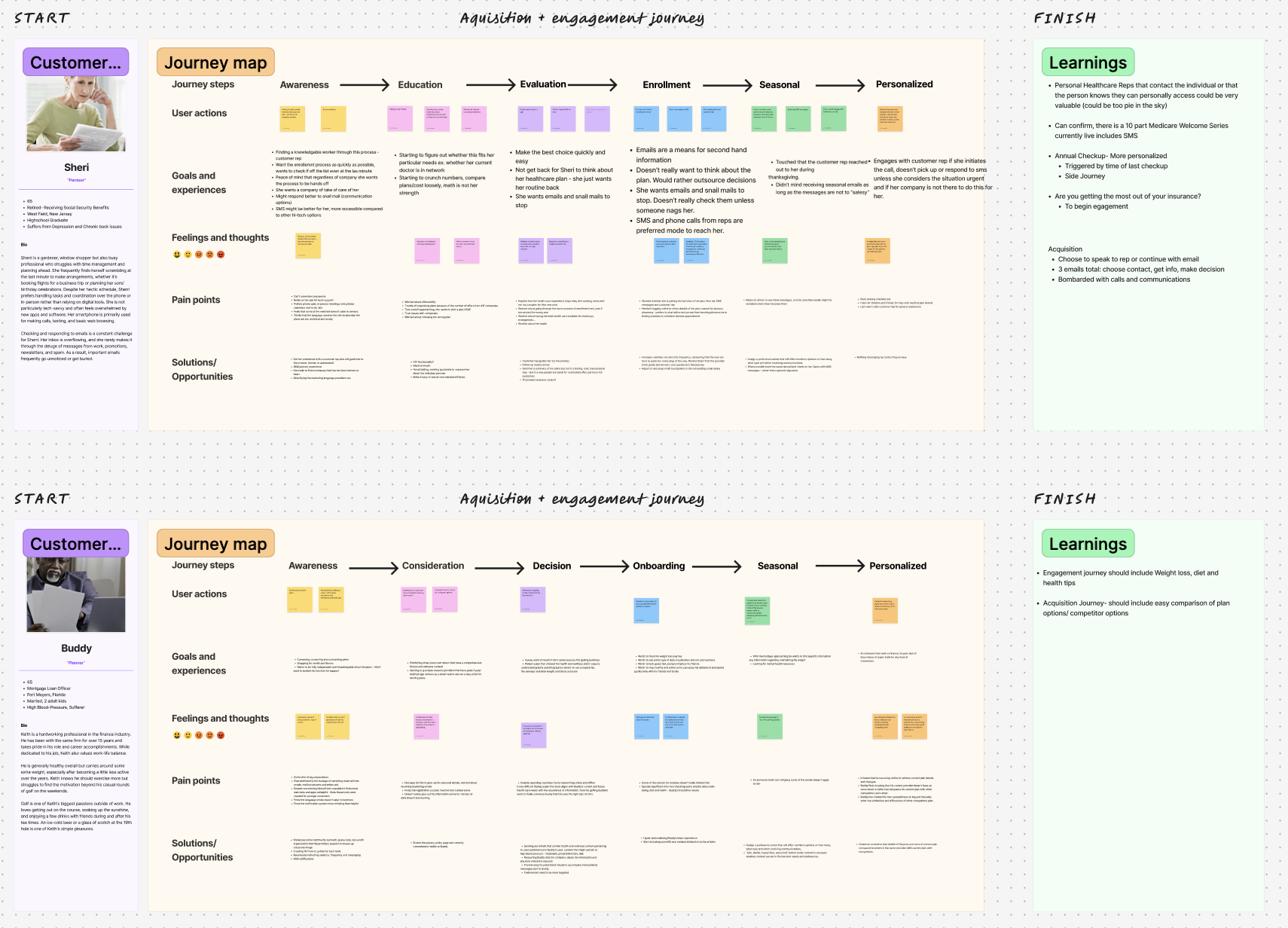
To get to the heart of the problem, I started with a full audience persona assessment. I wanted to go deeper than general demographics and really understand the pressures, worries, and motivations behind each click. We decided to split the audience into two groups – “planners” and “pantsers” (who fly by the seat of their pants) – for the initial journey send until we could glean more data and test into multiple audience segments.
There were Medicare shoppers who felt overwhelmed by the process, unsure how to choose a plan or who to trust for guidance. Then there were those who were engaged with the process, but wanted to ensure they were making the right choice. And behind both groups were the realities of busy, complicated lives: people balancing family, work, tight budgets, and their own health needs.
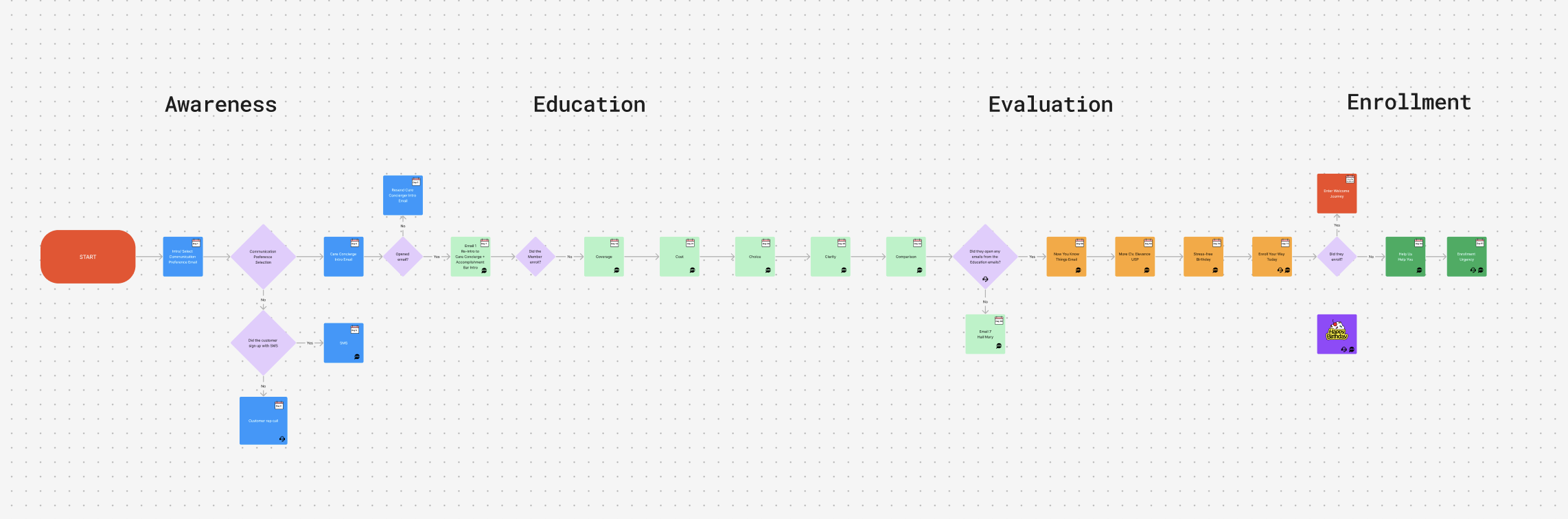
With that insight, I developed a content journey designed to mirror the way people naturally make decisions. It moved step by step, carrying them through awareness (“we see you, this is confusing”), into education (“here’s what this means for you”), on to evaluation (“why Elevance is the partner you want”), and finally to enrollment (“we’ll help you every step of the way”). We even planned to send a birthday celebration message with no associated enrollment push, just to help build a human relationship with shoppers.
The focus wasn’t on pushing plans. It was proving Elevance as a trusted resource.
Plain talk over corporate-speak, every time.
For the language itself, my guiding principle was simple: no jargon, no lectures. Just real, human conversation. Healthcare marketing is often cold and corporate, and Medicare enrollees were already receiving countless communications about their eligibility. These communications needed to feel like a helpful friend explaining something complicated in a way that actually made sense.
The copy mirrored the evolution of the client’s felt need as they learned more and as their enrollment deadline approached. We positioned Elevance not as a company selling coverage, but as a partner showing up with resources, clarity, and compassion.
A ready-to-launch journey strategy
(and a client that felt seen)
Before approaching the build stage, Elevance had to put the project on pause due to internal restructuring. While we didn’t get the chance to see the journey go live, the feedback we received told us we were on the right track. The client appreciated how we prioritized understanding their audience before writing a single line of copy.
What they valued most was the way we simplified a complex process while showing empathy for the people on the receiving end. It wasn’t just about insurance, it was about trust.
Whenever Elevance is ready to activate the journey, they’ll have a strategy in place that feels like a friendly hand extended to each enrollee, not just another marketing email landing in a crowded inbox.